Background: Myelofibrosis (MF) is a clonal myeloproliferative neoplasm characterized by hyperactive JAK-STAT signaling, bone marrow fibrosis, extramedullary hematopoiesis and splenomegaly. Ruxolitinib (RUX) and Fedratinib are both JAK inhibitors used for the treatment of patients with intermediate or higher risk MF. While RUX is the first line treatment for patients with MF, about 50% of the patients discontinue treatment due to lack of efficacy or intolerance (Harrison et al., Ann. Hematol. 2020) after 3 years. Fedratinib is used as a second line therapy in MF based on efficacy from the JAKARTA2 study. The recently concluded FREEDOM and FREEDOM2 studies further support this. In this work, using in vitro approaches, we have explored the mechanistic basis of fedratinib's ability to overcome RUX resistance.
Pharmacologically, Fedratinib binds with high affinity to the substrate-binding site and with low affinity to the ATP-binding site of JAK2(Kesarwani etal., Sci. Rep. 2015) while RUX binds only to the ATP-binding site. Previous studies on RUX resistance have shown acquired mutations driving resistance to RUX but not to Fedratinib. Here, we use RUX sensitive and resistant BaF3 (expressing human JAK2 WT or V617F) cell lines to examine the mechanism of resistance to RUX and the mechanism of efficacy of Fedratinib in RUX resistance.
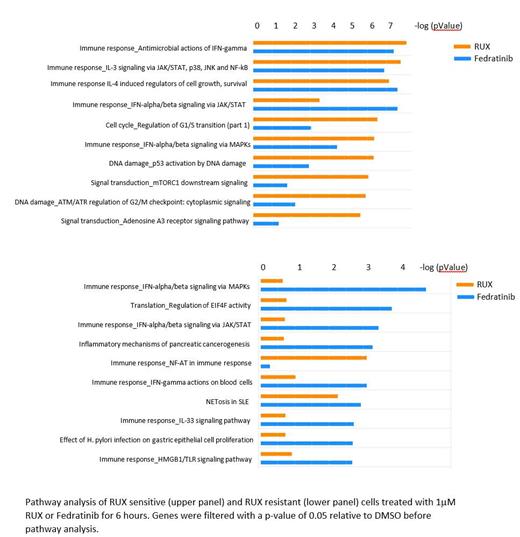
Methods: BaF3 cell lines overexpressing JAK2 WT or JAK2 activating mutation V617F were incrementally exposed to RUX over 3 weeks (up to IC 90) to induce resistance. Cell proliferation and phosphorylation of STAT5 in Fedratinib and RUX-treated cells were measured using celltiter glo and immunoblotting, respectively. RNAseq and ATAC-seq analyses were performed in triplicates by treating the relevant cell lines with DMSO, RUX or Fedratinib at two timepoints (6 and 15 hours). Pathway analysis was performed on RNAseq data using Metacore®.
Results and Discussion: Ruxolitinib resistant BaF3 JAK2V617F cells showed minimal inhibition of proliferation (<10%) when treated with RUX but maintained sensitivity towards Fedratinib (IC 50 650nM vs 1552nM in RUX sensitive and resistant cells respectively) in 24-hour proliferation assays. Biochemical analysis revealed that Fedratinib inhibited JAK-STAT signaling in the RUX resistant cell line while RUX was unable to do so as measured by p-STAT5. Similar results were observed in BaF3-JAK2-WT cells as well.
To further understand the mechanism of RUX-resistance and differential activity of RUX and Fedratinib, we performed RNAseq analysis on our RUX sensitive and resistant models before and after RUX and Fedratinib treatment. Myelofibrosis is associated with aberrant cytokine production and pro-inflammatory signaling that are mediated through activation of TNF-α and NF-κB signaling (Dunbar et al., Blood 2023). Consistent with this, RNAseq analysis of BaF3 JAK2 V617F cells treated with RUX or Fedratinib showed effective inhibition of these pathways by both agents as early as 6 hours. In the RUX resistant cells, while RUX did not have any significant pathway level changes, the top enriched pathways upon treatment with Fedratinib were predominantly interferon signaling pathways which includes JAK-STAT signaling suggesting that Fedratinib's efficacy in MF is not impacted by RUX resistance.
To understand the mechanism of resistance, comparison of gene expression data from RUX senstive and RUX resistant cells without any drug treatment revealed minimal gene expression/pathway level differences suggesting that the mechanism of resistance could be driven by genetic (Downes et al. NPJ Precis Oncol, 2021) or epigenetic changes(Dunbar et al., Blood 2023). Ongoing analyses includes whole genome sequencing and ATAC-seq to investigate potential mutations and chromatin accessibility changes during resistance acquisition to RUX and how Fedratinib may overcome these.
Conclusion: Our stable RUX resistant preclinical model demonstrates that Fedratinib is effective in overcoming RUX resistance by continuing to target key pathways in MPN biology including interferon signaling. Resistance to RUX on the other hand seems to be driven through potential genetic or epigenetic changes based on the minimal changes observed in gene expression profiles. Our ongoing analyses will reveal these potential genetic and epigenetic modifications associated with RUX resistance and explain the differential activity of RUX versus Fedratinib.
Disclosures
Jeyaraju:Bristol Myers Squibb: Current Employment, Current equity holder in publicly-traded company. Polonskaia:BMS: Current Employment, Current equity holder in publicly-traded company. Hsu:BMS: Current Employment, Current equity holder in publicly-traded company. Hagner:BMS: Current Employment, Current equity holder in publicly-traded company. Gandhi:Bristol Myers Squibb: Current Employment, Current equity holder in publicly-traded company.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal